“The first lesson I learned is how dumb I am. A year and a month ago, given the oxygen saturation levels we were seeing, I couldn’t have imagined not intubating people. We in Iowa got to learn from our confreres in New York and benefit from the pain and suffering of people there.
“This is stuff your mother taught you – wash your hands! Don’t spit on people! These simplistic lessons kind of got lost in all the technology. It’s like telling a 16-year-old: ‘You’re going to get your driver’s license, so I’m going to give you a new car, with only a few miles on it from the dealership. It will be pristine. But the caveat is that it’s the only car you will ever have.’ You would take great care of that car. That’s how we need to take care of our bodies. The virus doesn’t know squat; it doesn’t know the seasons. We do, and we can avoid some risks with our behaviors.”

“Telemedicine is the silver lining on the heavy cloud of the pandemic, which forced us to think outside of the box. We also tailored our triage process based upon the patients’ symptoms so that it’s safer. The use of Zoom in medical education also shifted the paradigm to a hybrid that I don’t think is going to go away.
“Hindsight is 20/20, but I wish that physicians would have had a louder stance early in the pandemic. We shouldn’t be a third world country, with so many resources, to be first in the number of deaths from COVID-19.
“I always communicate to our residents that this is the time they will look back on what they wrote in their personal statement to get into medical school, which typically relates to how they want to affect change in a positive way. These medical students saw a completely different side of medicine.”

“The pandemic shut everything down on a Friday; I started my new job the following Monday. Probably the hardest piece was trying to ensure calm within our team and keep everyone safe. They didn’t know me, and I was trying to learn everyone’s name. We made an immediate overnight shift with an incident command team that brought everyone together. It was important that our people felt safe, their voices were being heard and their families were being taken care of, including mentally. It was a huge reminder that it doesn’t matter if there’s a pandemic or flu outbreak; you just have to be sure you’re giving your team what it needs.
“Supply procurement has been a huge lesson learned for everyone in health care – anticipating needs and making sure we have enough supplies to get us through.
“One thing we did really well was to ramp up communication among all employees. Starting in April [2020], I made a weekly recording on an iPad that everyone received on what was happening with COVID-19 and what we were doing. That was challenging since every day was different and sometimes things were changing by the hour, but you have to roll with the punches.”

“The pandemic brought different groups together that hadn’t worked together before. We developed rapport with our schools and had more interaction with hospital systems, infectious disease doctors, long-term care facilities, laboratories and other organizations. We worked with people in social services to help people in their system who are experiencing homelessness, who are addicted and who were COVID-positive who needed services.
“I hope we continue to enhance surveillance and our data analysis systems. I hope it’s not just one bolus of ‘Yay, public health!’ and then that support goes away.”
Emily Hanlin, M.P.H.’20, is an infectious disease epidemiologist at the Delaware Department of Health and Social Services in its public health division. During the pandemic, she has focused on COVID-19 case investigations and contact tracing as well as monitoring vector-borne diseases and tuberculosis. Her master of public health capstone project was on the implementation of a molecular epidemiology program for epidemiologists in Delaware, using genetic sequences to infer whether infectious disease outbreaks or clusters are related.

“I never thought my name would be on a letter to Nancy Pelosi. As members of the American College of Foot and Ankle Surgeons, we asked to be put on the front lines for COVID-19 treatment if our help was needed. The pandemic taught us to be open to change and adaptable and to accept the fact that nothing is constant.”
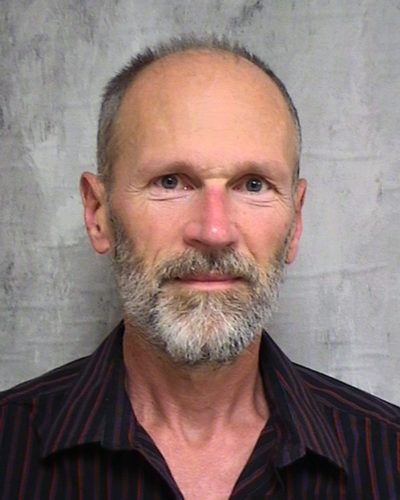
Scott Nelson, D.P.M.’00, FACFAS, is a foot and ankle surgeon with the CHI Health Department of Orthopedics in Omaha, NE; immediate past president of the American College of Foot and Ankle Surgeons; and the 2020 College of Podiatric Medicine and Surgery Alumnus of the Year.
