General information on pelvic health for males is more difficult to find than for females, and guys certainly don’t sit around the coffee shop talking about their urinary incontinence after having prostate cancer. However, information should be available since prostate cancer happens in 1 out of 7 males and 80% affected will be incontinent after a radical prostatectomy, many times remaining incontinent after a year. The disclaimer here is although many men do not consider “a little dribble” or “a little squirt after standing” as incontinence, 80% of males post radical prostatectomy will have those symptoms and greater involuntary urine leakage.
It has been a year since my father was diagnosed with prostate cancer and had a prostatectomy for treatment of the metastasis. I was able to experience first-hand the journey he went through from the delayed access to care (three months wait to get to urology), diagnosis, treatment, and the struggle to regain continence. The impact it had on his quality of life and mental health made this hardworking, 83-year old farmer slow down more than the heart surgery or subdural hematoma he had years earlier.
What’s involved in an incontinence treatment plan?
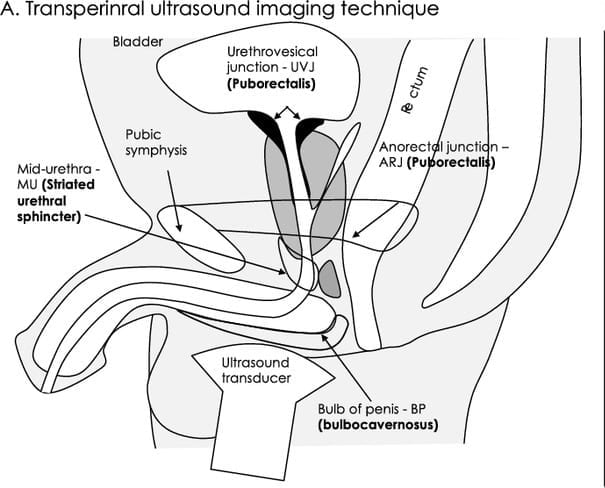
I am a pelvic floor physical therapist and treat men, women, and children with incontinence (along with many other diagnosis). The American Physical Therapy Association’s Pelvic Health Academy has been advocating for “prehab” or a single session with patients prior to having the prostatectomy, much like an orthopedic patient has a PT session before hip or knee surgery in order to understand the rehabilitation of the pelvic floor post-surgery. The surgeon informs the patients about what to expect medically and may give them a handout on Kegels or pelvic floor exercises, and off they go to surgery to remove the cancer and get back to normal life. In my experience, my father and all patients I have seen, do not understand how to contract the pelvic floor muscles to have fewer symptoms of incontinence afterwards. Patient handouts are often geared toward females, but the anatomy and continence mechanism are significantly different in males. Research (3,4,5) shows that to remain continent after radical prostatectomy specific muscles must be activated: the striated urethral sphincter, bulbocavernosus and puborectalis muscles. These muscles are different than the muscles that are the focus in most patient handouts. Activation requires specific instruction and feedback for success. Generalized instructions to “hold back gas” or contract around the anus will not activate these specific muscles.
What can I expect during my first pre-surgical evaluation?
During an evaluation with a pelvic floor physical therapist, a review of your overall health is performed along with a detailed history of continence status through a questionnaire, review of activities that cause leakage, and bladder habits. An assessment of the ability for the trunk and pelvic muscles to maintain continence during daily functions is performed. The exam may include palpation of the pelvic floor muscles (particularly the bulbocavernosus) externally or rectally to determine the tone, strength, and functional capacity of each muscle; these muscles have an impact on the striated urethral sphincter and subsequent continence in men.
Seeing a patient before radical prostatectomy allows the PT to teach them how to optimize the contraction of the pelvic floor muscles with bias toward the striated urethral sphincter. This allows for the cognitive learning process of muscle awareness during conscious practice to visualize stopping the flow of urine or retracting the penis. It is more difficult to teach this learning post-surgically, when patients are sore, muscles are deconditioned and incontinence is evident. Once pelvic floor activation is achieved, integrating the pelvic floor contraction into function—such as pre-contracting the pelvic floor as you move from sit to stand—is important. Post-surgically, after the urinary catheter is removed, these exercises can be resumed. After surgery, pelvic physical therapy includes working on endurance of the pelvic floor and maintaining continence with movement and leisure activities.
What can I expect after surgery?
Bladder training also will occur post-surgery. Reducing fluid intake is a common patient response to incontinence. It seems to make sense, drinking less should cause you to have less urine and going to the bathroom more frequently should reduce the incontinence. Unfortunately, it’s not so simple; in fact, increasing voiding frequency often reduces the bladder’s ability to hold urine adequately without becoming incontinent. Maintaining bladder compliance with adequate filling and time between voids is a goal to return to normal bladder function. Many people do not get adequate hydration, so never try to restrict fluids to prevent leakage. Your body needs water!
Recovery after surgery
Optimal recovery from prostate cancer and incontinence requires adherence to a pelvic muscle exercise program along with other health and wellness strategies. Managing bowel consistency will impact continence, and maintaining positive mental health practices helps avoid frustration or depression as the client goes through this scary and life-changing diagnosis. Participating in a general exercise routine improves strength and function throughout the body and weight maintenance allows the pelvis to heal without the stress of increasing body mass. Sexual dysfunction and/or erectile dysfunction are common with radical prostatectomy. Pelvic physical therapy can also provide strategies for management, so if you have questions ask your health care provider. Urinary incontinence in men is common after prostate cancer treatment.
If you are preparing to have surgery or are experiencing incontinence, you don’t have to suffer in silence. The Des Moines University Clinic has exceptional physical therapists who specialize in pelvic health for both men and women. Schedule an appointment at 515-271-1717 or visit the DMU Clinic website for more information.


