The team’s patient, Harriett, was a 67-year-old woman who had been brought by ambulance to the rural hospital’s emergency room after a neighbor discovered she’d fallen in her home and was unable to get up. She had high blood pressure, diabetes, multiple bruises and no health insurance, but her biggest concern was returning home to check on her cat, Rusty. It was the team’s duty not only to diagnose and treat her conditions but also to determine follow-up care and, if possible, connect her with resources to enhance her health.

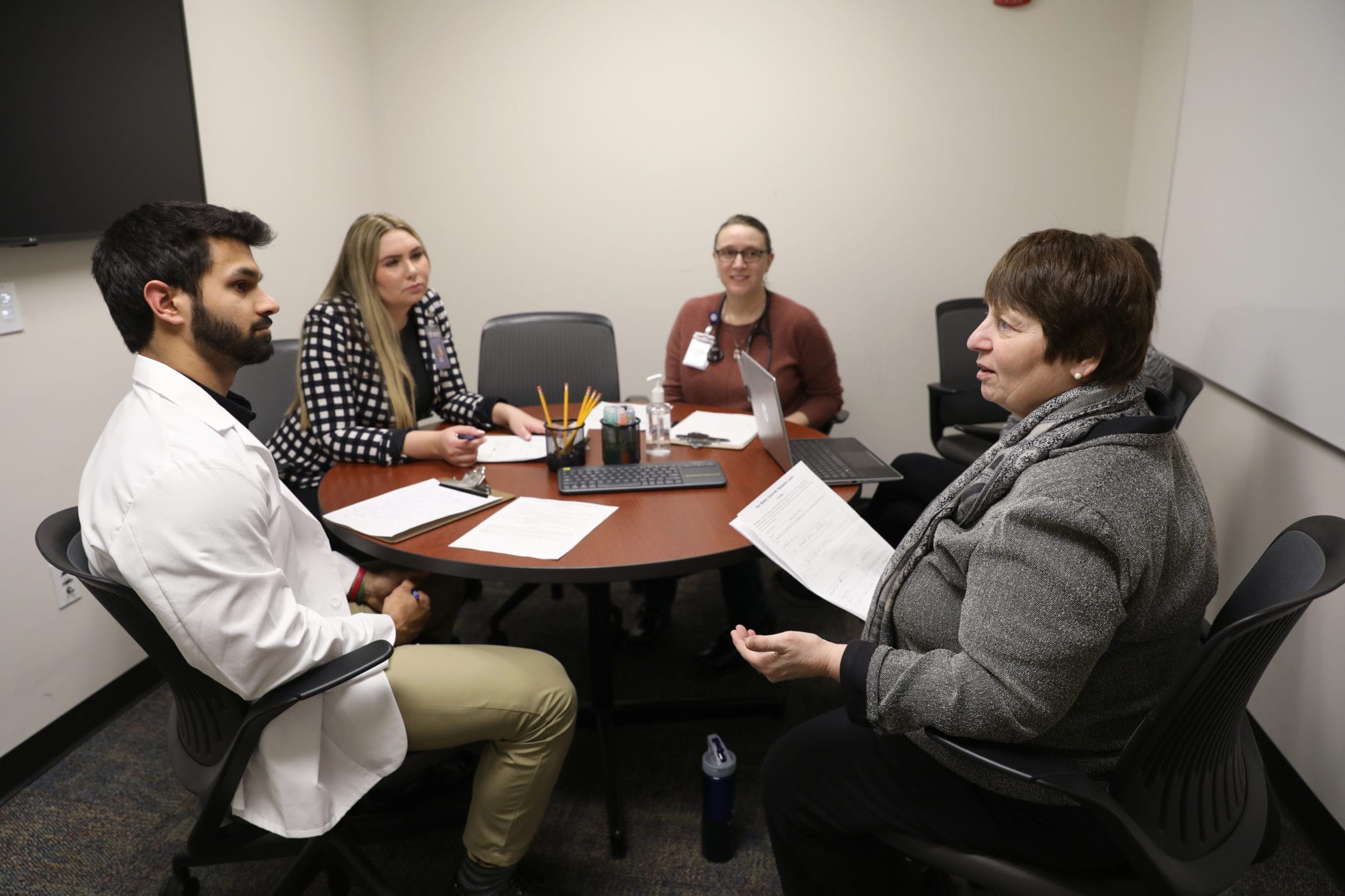
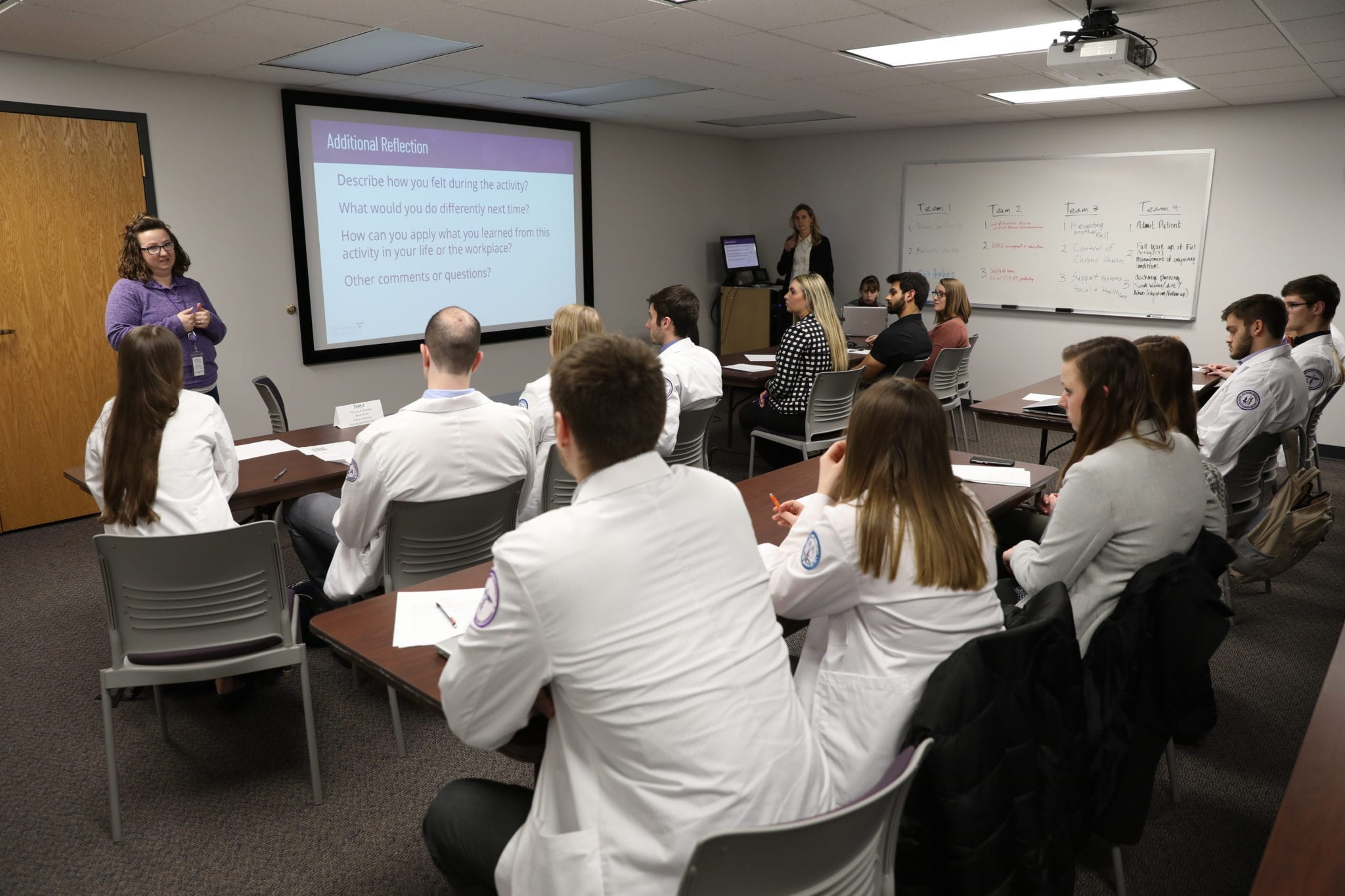
That was the scenario that 31 DMU first-year students participated in on a recent Friday afternoon in the University’s simulation center. Representing the osteopathic, podiatric, physician assistant, physical therapy and public health programs, the students had volunteered for the event to learn what it was like being on interprofessional health care teams. Faculty members guided their discussions in an orientation session, observed their interactions with the patient and then led a debriefing. Their “patients” were community members who served as “standardized patients,” trained to depict the conditions presented in the case.
The objectives were for students to understand their own and other team members’ roles, experience the benefits of interprofessional teamwork to patients and then consider additional team members and health services that could be part of the patient’s care.

Students also considered the realities of rural health care settings, such as limited resources and patients who skew older and who may put off preventive care, who prefer to age in their homes and who may not understand how to manage their health conditions.
The simulation exercise stimulated lively discussions. Students talked about not wanting to “step on the toes” of their teammates while questioning the patient. They explored resources to suggest for Harriett, such as getting her information about Medicare, having her talk with a dietitian at her local grocery store and getting her a monitor she could wear in case she fell again. A public health student said Harriett’s comments about the high cost of her medications made her think about obstacles to good care presented by the nation’s health care system. Physical therapy students were praised for asking about Harriett’s home set-up and exercise routine but acknowledged they knew less about medications than did the osteopathic and physician assistant students.

Students also talked about how they could have been more empathetic to the patient and ways to optimize the knowledge and expertise of each team member.
“As students interact with standardized actors who realistically present as the patient in this case study, students develop their own communication skills so important to successful teamwork – listening to the patient and listening to each other,” emphasizes Pamela Duffy, P.T., Ph.D., FAPTA, associate professor in DMU’s public health department, one of the faculty members who led the orientation and debriefing sessions.
The exercise represents the University’s overall effort to integrate interprofessional education into students’ curriculum and co-curricular activities through a pilot program as part of the Higher Learning Commission’s Assessment Academy.
“This event is part of a two-year sequence of interprofessional education opportunities available to first- and second-year DMU students that began with an orientation to IPE in July,” says Amy Morris, Ph.D., M.S., assistant provost of accreditation and quality improvement.
The Institute of Medicine, the World Health Organization and many other organizations support interprofessional learning among future health care professionals to enhance patient care and safety, decrease costs, reduce medical errors and achieve other benefits. Interprofessional interaction also better represents the types of settings in which most students will go on to work.
“We are educating our students to be change agents in the health care system and to go out and create interprofessional teams in their practice settings,” Dr. Duffy says.

